Medication-assisted treatment (MAT), including Methadone, Buprenorphine, and Naltrexone, has been clinically proven to reduce opioid use. However, we’ve heard from community members across Ohio that it’s difficult to find treatment providers, especially in rural areas. In 2018, increased federal funding, outreach programs, and legislation are aiming to increase the amount of treatment centers and training for prescribers across the state. In this week’s blog, we take a look at the history of MAT access, and how prescribing guidelines are beginning to change.
Getting a prescription
Most people are familiar with some forms of medication-assisted treatment. Here’s a brief overview of the three major kinds, and how they are currently prescribed, according to the Rural Health Monitor:
- Methadone: this drug is prescribed through a methadone clinic, which are specialized centers that must receive special federal approval to prescribe regulated opioid treatment. Note: prescribers can get a special license to prescribe methadone for other things, like cancer pain.
- Buprenorphine: to become a buprenorphine prescriber, you must take an eight-hour training course, then apply for a DEA waiver to begin prescribing. This process can take up to 45 days. While special permission can be granted for more immediate prescribing, the provider must be licensed, have a DEA registration, and have completed training.
- the 2016 Comprehensive Addiction and Recovery Act (CARA), granted nurse practitioners (NPs) and physician assistants (PAs) to also become prescribers of Buprenorphine, to help in rural and underserved areas. These providers can also obtain waivers, but need to undergo 24 hours of training instead of 8.
- Naltrexone: this treatment has been clinically tested less than the others above, can be prescribed by any treatment provider.
Most experts see MAT as most effective, according to the Substance Abuse and Mental Health Services, when used “in combination with counseling and behavioral therapies.”
Availability of Treatment
A series of maps published by amfAR earlier this year shows the availability of facilities that treat substance use disorders, the facilities that provide at least one form of medication-assisted treatment, and the facilities that provide all three kinds of medication-assisted treatment for opioids. Only 2.7 percent offered all three.
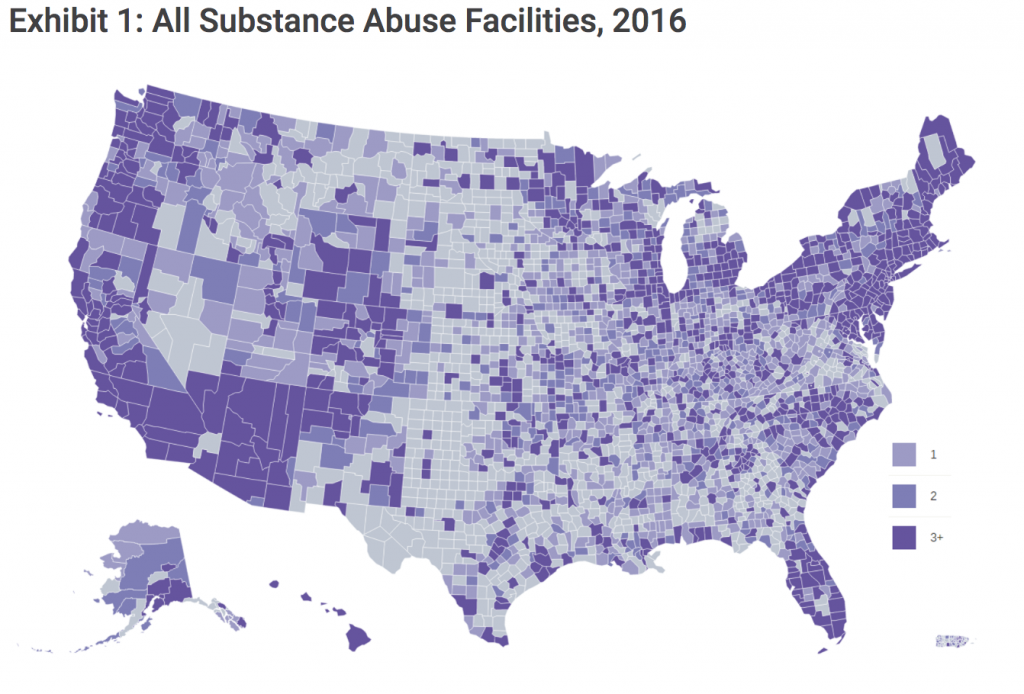
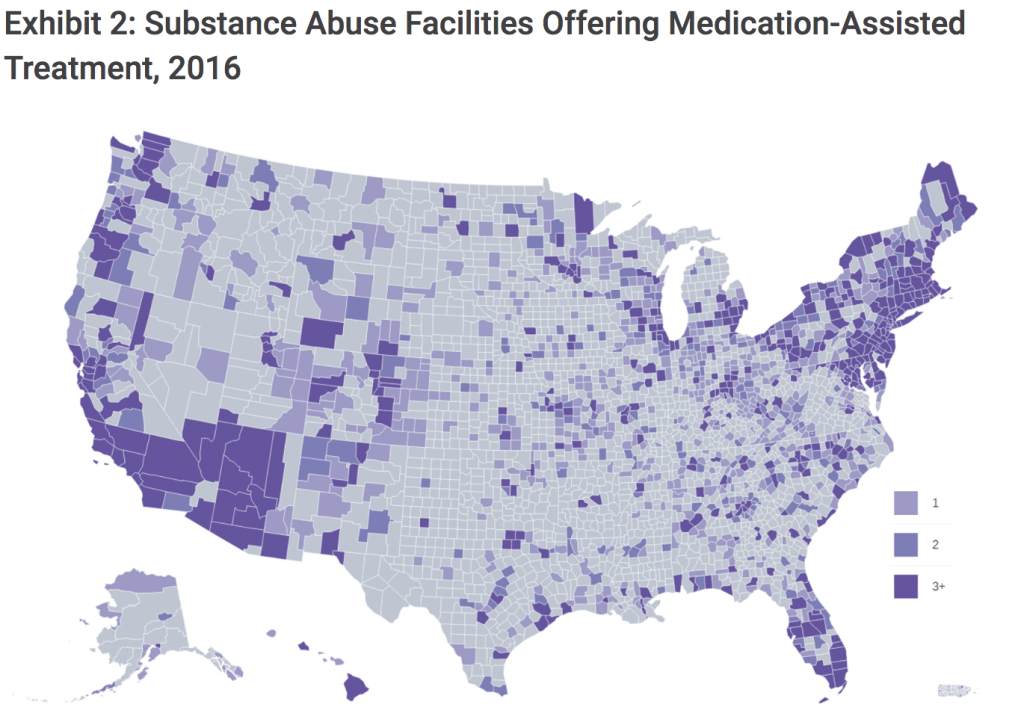
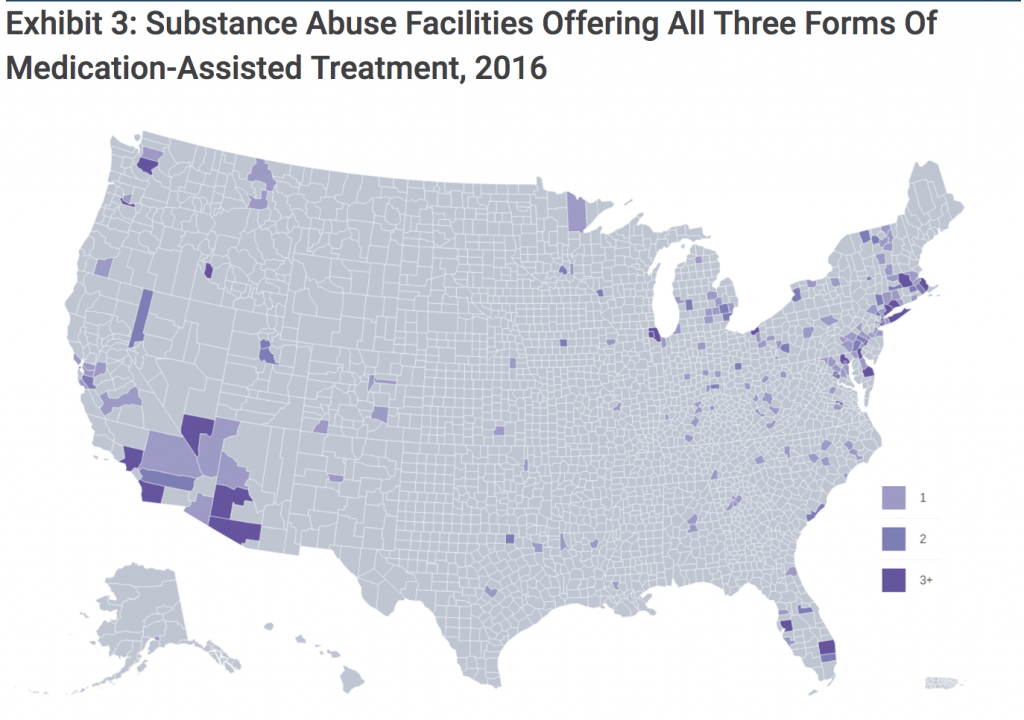
These maps highlight “significant gaps in access to MAT and in particular extremely low availability of all-MAT facilities in most of the country,” write the authors of the study in Health Affairs. Especially in the central United States, including areas particularly hard-hit like Tennessee, Ohio, and Kentucky, access to treatment is further limited when facilities don’t accept Medicaid.
Although healthcare facilities in rural and underserved areas may be able to prescribe MAT, through trainings, waivers, and by getting federal approval, this doesn’t always happen. A study from the WWAMI Rural Health Research Center found three major challenges that rural prescribers face:
- Time constraints
- Lack of behavioral health and psychosocial support services
- Concerns about drug diversion and medication misuse
Increased Funding
A few different grants aim to expand MAT access, research, and advocacy. States, territories, and jurisdictions can apply for the Substance Abuse and Mental Health Services Administration (SAMHSA) State Targeted Response to the Opioid Crisis Grants. Grant awardees are selected via formula based on current “unmet need for opioid use disorder treatment and drug poisoning deaths”
These SAMHSA grants, over the past year, have added a total of 266 new providers across Ohio who are trained to prescribe buprenorphine, reports Cleveland.com. At the beginning of 2017, 1,100 doctors (about 2% of the physician workforce), were licensed to prescribe the medication. Already in February 2018, 140 more doctors completed the training and applied for a DEA waiver to immediately begin prescribing. These numbers will likely continue to increase with the help of $2.3 million dedicated to training, part of a wider $52 million grant from SAMHSA to boost the number of patients who can access treatment statewide.
Legislation
A bill called CARA 2.0 is in the early stages of the legislative process, and would make Section 3 of the original Comprehensive Addiction and Recovery Act (CARA) permanent: physician assistants and nurse practitioners could continue to prescribe buprenorphine under the direction of a qualified physician. The bill would also allow states to waive the limit on the number of patients a physician can prescribe buprenorphine, as long as they follow strict guidelines. Currently physicians can prescribe up to 100 patients buprenorphine at one time. This bill has bipartisan support, according to the Washington Court House Record Herald, including from U.S. Senators Sherrod Brown and Rob Portman.
As the Portsmouth Daily times reported last week, Senator Portman and Bob Casey (D-PA) introduced the Medicare Beneficiary Opioid Addiction Treatment Act (S. 2705), that would provide coverage for methadone under Medicare Part B. This would allow seniors and people with disabilities to receive methadone at their doctor’s office. As we found in our insurance coverage blog, methadone can’t be dispensed in a retail pharmacy, which can cause complications for patients. This legislation may shift the attitude towards elderly patients that use MAT: Stat news reports, “Nursing facilities routinely turn away patients seeking post-hospital care if they are taking medicine to treat opioid addiction.” In Ohio, a trade group representing more than 900 facilities said in a written statement in 2017 that none of its member facilities will accept patients who receive methadone or buprenorphine.
How to find treatment
If you are seeking MAT for yourself or a loved one, SAMHSA’s buprenorphine treatment practitioner locator is a good place to start. It provides locations of physicians authorized to treat opioid dependence with buprenorphine by state. There are 53 pages of people to contact just in Ohio, including both medical doctors and nurse practitioners. Otherwise, connecting with your local Alcohol, Drug Addiction and Mental Health Services (ADAMHS) Board or confidentially calling the Substance Abuse and Mental Health Services helpline should be able to point you towards the right resources.
Many communities may not support the use of MAT simply because we don’t often see the success stories of treatment. Here are few programs beginning to take shape in Ohio:
- In Fayette County, Vivitrol (Naltrexone) is offered in combination with counseling. The Vivitrol program is billed through the patient’s insurance. Patients who do not have health insurance are referred to locations that offer Vivitrol on a sliding scale fee based on income, reports the Washington Court House Record Herald.
- Hancock County is expanding MAT treatment for youth.
If you or someone you know has used MAT to treat opioid use disorder, and you’d like to share your story, you can contact us here.
MAT Risks
Many people are hesitant when it comes to supporting MAT. Some question the short term versus long term recovery effects. Others tend to view the treatment as a trade-off, writes German Lopez, who has been following the crisis closely for Vox: “These medications are often characterized as “replacing one drug with another” — say, replacing heroin use with methadone use.” We’ve heard similar sentiments in our community meetings, where often times people who have worked through recovery without the use of MAT feel that it’s unnecessary, and even enables the person in recovery.
In an interview with the Youngstown Vindicator, Girard resident Alexis Graziano, who is half a year into recovery, said, “MAT only delays facing up to the reality of it will take to get better.”
For more research about the research and effectiveness of MAT, check out our story: Medically Assisted Treatment: what’s healthy, effective, and affordable?
We recognize people have varying opinions and experiences with MAT, and we want to know your thoughts. Let us know below. To follow our new research and research of our local media partners, sign up for our weekly news roundup.

I have been a counselor in Mat program for years and I have seen much success with my clients I am happy to hear that there is support for these programs
As long as a patient has access to any opioid that is pharmaceutical quality and affordable,it’s not a huge feat to have a life that is as normal as anyone taking medication such as insulin. The problems occur because of black market prices and unpredictable quality. You’ve probably been working with many people who have been taking opiates for years to treat back pain or neuralgia. They just don’t have to spend all their money on their script. They’d look like the average junky in a month if their meds started costing $100 a day just to get enough to sleep and eat and function. The damn laws need changed. Fentanyl is the easiest thing on earth to traffic. It’s here to stay. Make access to poppies legal and it will disappear overnight.