We have previously explored how people can become chemically dependent on opioids, and it’s important to note that there are also a number of risk factors that have been found to lead to a higher likelihood of drug use. It is possible for some people to be more susceptible to becoming addicted than others, depending on various genetic, biological, and environmental factors. One of these factors has been found to be mental health.
The Issue
A 2017 study found that 81 percent of those whose addiction began with chronic pain, also had a mental health disorder. A 2012 survey found patients with depression were twice as likely to misuse their opioid medications. When someone with a mental health issue takes an opioid for physical pain, it also relieves their emotional distress. However, this can be dangerous because repeated exposure to escalating doses of opioids alters the brain so that it functions more or less normally when the drugs are present and abnormally when they are not; leaving people to associate the drug with positive emotions, and may eventually have trouble feeling well without it. This compound the effects of physical dependence, making it especially difficult for them to recover.
Another study found patients on morphine experience 40 percent less pain relief from the drug if they have a mood disorder. This suggests that not only does a mood disorder affect a person’s potential for addiction, but it also has an impact on the ability of the drug to successfully treat their pain.
Furthermore, voluminous research conducted over the last two decades indicates that mental health tends to decline during periods of economic weakness. One study found that as the county unemployment rate increases by one percentage point, the opioid death rate per 100,000 rises by 0.19 (3.6%) and the opioid overdose ED visit rate per 100,000 increases by 0.95 (7.0%).
The Treatment
Dual diagnosis is the term used when a person has a mood disorder and a substance use disorder. A person who has a dual diagnosis has two separate illnesses, and each illness needs its own treatment plan. According to a 2014 National Survey on Drug Use and Health, 7.9 million people in the U.S. experience both a mood disorder and substance use disorder simultaneously. More than half of those people—4.1 million to be exact—are men.
One of the things that make dual diagnoses so difficult to treat is that it is hard to know where certain symptoms are coming from. That is why the best dual diagnosis programs provide integrated treatment – treating and addressing both the mental illness and the substance use at the same time all under “one roof”.
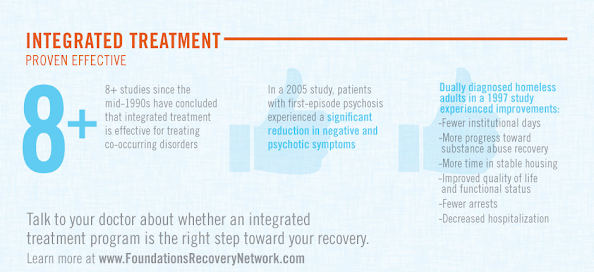
Treating both disorders at the same time is often effective because of the ways that these conditions interact with each other. If one disorder is left untreated, it can worsen and negatively affect any progress made to treat the other disorder. Additionally, the two conditions may be related to each other in complex ways, so treating them simultaneously offers the person the best opportunity to address these relationships and figure out how best to manage both disorders on a daily basis.
Despite increased awareness of the benefits of integrated services for persons with co-occurring substance use and psychiatric disorders, access to integrated services vary widely. Find out what integrated treatment service exist near you here.